Salmonella bacteria have been isolated from nearly all vertebrates, and infections have been associated with both animal and human disease. Not uncommonly, foods of animal origin have been implicated as the source of human illness caused by salmonella. Typical signs of salmonella infection in cattle and humans include fever and diarrhea. Severe cases can result in death.
Shedding of salmonella bacteria in both beef and dairy cattle often occurs in the absence of clinical signs — sometimes for extended periods. Once infections are established, treatment and elimination of infection is often difficult. Latent (subclinical) infections often become evident during periods of stress, like calving season.
Read Also

Canadian Beef Check-Off Agency reports on investments and activities
The check-off agency’s work behind the scenes is what ensures cattle check-off dollars are invested wisely, accounted for transparently and deliver measurable value back to producers and importers.
Salmonellosis in humans is typically self-limiting and most people recover within one week, but they too can become asymptomatic carriers, excreting large numbers of bacteria in their feces and contaminating food and water sources. What first appears as a simple, perhaps unusual event in the calving barn, may be the precursor to a major disease outbreak affecting both humans and animals.
Salmonella organisms spread directly from contaminated surfaces and instruments, from an infected animal or human, or through food. Food contamination is not limited to products of animal origin. For example, fruits and vegetables irrigated with contaminated water are important sources of salmonella, if not washed properly or cooked prior to consumption.
Salmonella resistance to antimicrobials is a serious concern in severe infections when they are called for. Multi-drug resistance complicates and narrows treatment options.
The U.S. Department of Agriculture’s National Animal Health Monitoring System (NAHMS) conducted the Beef 2007-08 study, capturing information on beef cow-calf health and management practices in 24 states representing nearly 90 per cent of U.S. beef cows. The 2007-08 study paralleled a similar survey from 1997. Approximately, 10 per cent of the herds had at least one positive cow. Nearly one per cent of animals tested were shedding salmonella. The results suggest that salmonella, though not very common in beef cow-calf operations, exist undetected on a significant number of farms.
Biosecurity remains the single most important tool in reducing the risk of salmonella and other important calving shed zoonoses from gaining a foothold.
In September 2012, nearly 50 people in nine states became ill from eating ground beef tainted with salmonella enteritidis, according to the U.S. Centers for Disease Control and Prevention. In 2013, salmonella typhimurium in ground beef was linked to more than 20 human illnesses in six states.
Drug-resistant strains
Through 2016 and 2017, CDC, state governments, and the U.S. Department of Agriculture’s Animal and Plant Health Inspection Service (USDA-APHIS) investigated a multi-state outbreak of multidrug-resistant salmonella Heidelberg infections. A total of 54 people infected with outbreak strains of Salmonella Heidelberg were reported from 15 states. Thirty-five per cent of those infected required hospitalization. Thirty-three per cent of people involved were children under the age of five. No deaths were reported.
Epidemiologic and laboratory investigations linked ill people in this outbreak to contact with calves, including dairy calves. Ongoing surveillance in veterinary diagnostic laboratories showed that calves in several states continue to get sick with the outbreak strains of multi-drug resistant salmonella.
Information collected earlier in the outbreak indicated that a majority of calves came from Wisconsin. Investigation on new cases continues. Antibiotic resistance testing conducted by CDC on clinical isolates from ill people show that isolates were highly resistant to a broad spectrum of antimicrobials.
Through the years, salmonella outbreaks in Canadian beef and dairy herds have been reported. A 2003 Alberta study in dairy herds found the prevalence of salmonella similar to that found in the U.S.
Raw or undercooked poultry account for a large percentage of salmonella outbreaks in Canada.
Salmonella bacteria are found naturally in the intestines of domestic animals, reptiles and birds. The bacteria are most-often transmitted to people through contaminated foods or by handling animals shedding the organism. Contaminated foods often come from animal sources, like poultry, beef, milk or eggs, but also include fruits, vegetables, and herbs.
“It was always our working assumption that E. coli interventions [for cattle] should be controlling salmonella,” said James Marsden, a professor of animal science at Kansas State University. “E. coli is transferred from the beef hide to the carcass and works its way through the system. We thought this is what salmonella did as well. The incidences of E. coli have dropped sharply over the past 10 years, but salmonella isn’t dropping, which is perplexing,” Marsden added. “And some strains of salmonella that have been observed in beef are drug-resistant strains, so they pose a public health problem.”
Researchers at Texas Tech University now believe that, unlike E. coli, salmonella resides in the lymphatic system of cattle. “In 2010, the industry was in a position to start asking questions,” said Guy Loneragan, professor of animal science and lead researcher at Texas Tech University. “We started looking at the lymph nodes, which are internal and exempt from current prevention techniques.”
An August 2013 article published by the Midwest Center for Investigative Reporting by Sam Robinson, as part of a series titled “Cracks in the System,” called salmonella-tainted ground beef a major challenge facing the industry. Scientists have realized they may have misidentified the source of salmonella in beef cattle.
They now realize it may be in the lymphatic system of cattle, making it harder to prevent than E. coli.
Basic biosecurity precautions when working with livestock involve:
- Washing your hands thoroughly with soap and water after touching or treating livestock, handling equipment, or leaving areas where animals are housed. Adults should supervise handwashing for young children. Use hand sanitizer if soap and water are not readily available.
- Do not eat or drink in the areas where livestock are handled.
- Do not allow toys, pacifiers, spill-proof cups, baby bottles, strollers, or similar items in livestock areas.
- Use dedicated clothes, shoes, and work gloves when working with livestock.
- Keep and store these items in a separate area.
Biosecurity precautions are especially important in households with children under age five and around people with compromised immune systems.
Work with your veterinarian to develop animal health and biosecurity protocols.
Suspect salmonella cases involving adult cattle, or beef and dairy calves, especially those associated with human illness, should be reported to provincial government animal health or public health agencies. Salmonellosis is a notifiable/reportable disease in many provinces.
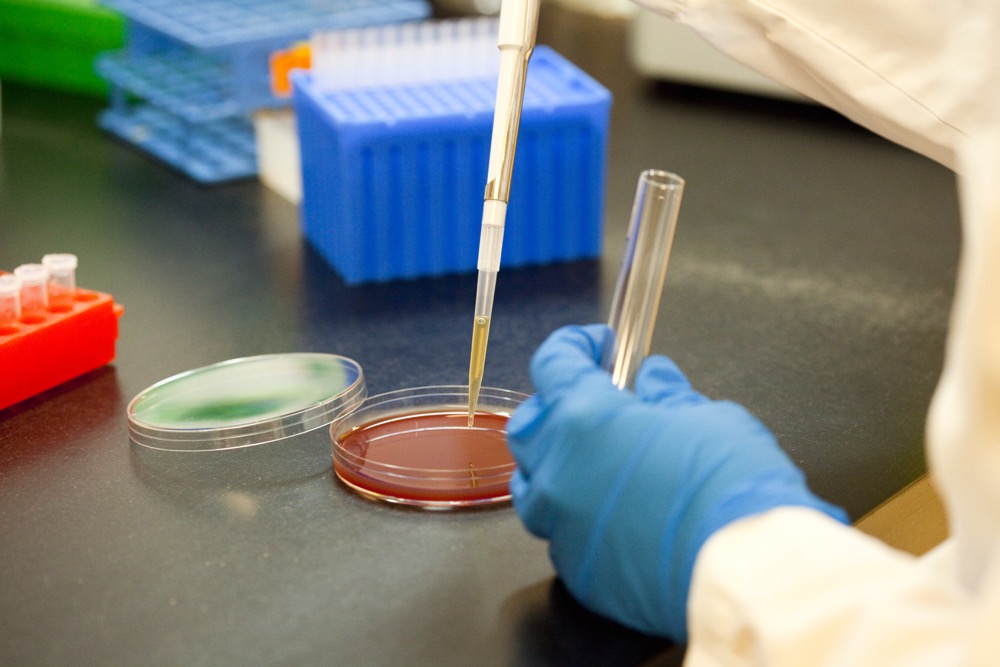
In the case of suspect salmonella infection, fecal samples are typically collected and submitted to a provincial or university veterinary diagnostic laboratory for culturing and pulsed-field gel electrophoresis (PFGE) testing.
Clients should talk to their veterinarian about reducing the risk of transmission of salmonella and other zoonotic diseases from livestock to their family.
Follow good food-handling practices (keep raw food away from other food while shopping, storing, preparing and serving foods; wash fresh fruits and vegetables before eating them, clean counters and cutting boards and wash hands regularly).
Keep pets away from food storage and preparation areas. Wash your hands well with soap and water after handling pet treats, pet food and pet toys, or after playing with or cleaning up after your pet.